Provider credentialing serves as the cornerstone of quality healthcare delivery, ensuring that healthcare professionals possess the requisite qualifications and competencies to deliver safe and effective care. In recent years, the landscape of provider credentialing has undergone significant transformations driven by technological advancements, changing regulatory landscapes, and evolving patient care models.
This article explores ten emerging trends in provider credentialing within the healthcare industry, highlighting innovations that are reshaping the way healthcare organizations verify, assess, and monitor the qualifications of their providers.
1. Digital Provider Credentialing Platforms
Healthcare organizations are increasingly leveraging digital platforms to streamline provider credentialing processes. These platforms offer centralized repositories for storing credentialing data, automating credential verification tasks, and providing real-time status updates on credentialing applications.
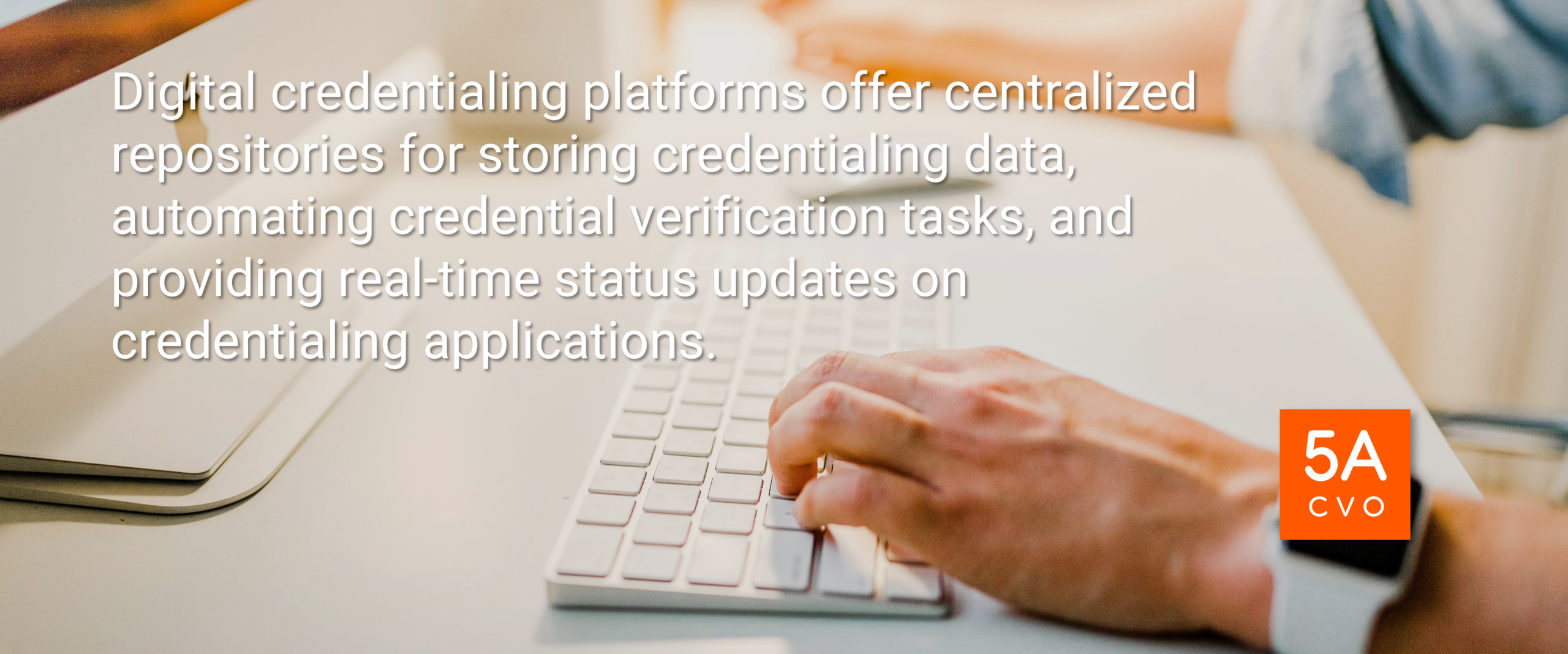
By digitizing credentialing workflows, healthcare organizations can reduce administrative burdens, improve efficiency, and enhance compliance with regulatory requirements.
Source: Healthcare IT news websites such as Healthcare IT News or industry reports from consulting firms like Deloitte or PwC often discuss trends in digital healthcare solutions.
2. Centralized Credentialing Services
Centralized provider credentialing services are gaining prominence as healthcare networks and managed care organizations seek to standardize credentialing criteria and processes. By consolidating credentialing functions under a unified framework, healthcare organizations can achieve greater consistency in credentialing decisions, enhance data integrity, and mitigate compliance risks.
Centralized credentialing services facilitate interoperability and data exchange between healthcare entities, fostering collaboration and information sharing.
Source: Industry publications such as Healthcare Finance News or academic journals in healthcare administration and management might contain articles discussing centralized credentialing trends.
3. Telehealth Credentialing Standards
The rapid expansion of telehealth services has underscored the need for standardized credentialing criteria for telehealth providers. Healthcare organizations are developing telehealth-specific credentialing standards to assess providers’ competencies in delivering virtual care.

These standards encompass areas such as technology proficiency, communication skills, and adherence to telehealth regulations. By establishing clear telehealth credentialing guidelines, healthcare organizations can ensure the quality and safety of telehealth encounters while promoting access to remote care services.
Source: Organizations like the American Telemedicine Association (ATA) or the National Committee for Quality Assurance (NCQA) frequently publish guidelines and standards related to telehealth.
4. Enhanced Verification Processes
Credentialing organizations are enhancing verification processes to validate the accuracy and integrity of provider credentials. Advanced verification methods, such as primary source verification and data analytics, enable healthcare organizations to verify education, training, licensure, certifications, and malpractice history with greater efficiency and accuracy.
By adopting robust verification protocols, healthcare organizations can mitigate credentialing fraud, minimize credentialing errors, and uphold regulatory compliance standards.
Source: The National Association Medical Staff Services (NAMSS) or the Joint Commission often publish articles and resources related to best practices in credentialing and verification.
5. Automated Credentialing Workflows
The provider credentialing process is so tedious that automation should be applied when possible. Automation technologies, including robotic process automation (RPA) and artificial intelligence (AI), are revolutionizing credentialing workflows by automating repetitive tasks and decision-making processes.
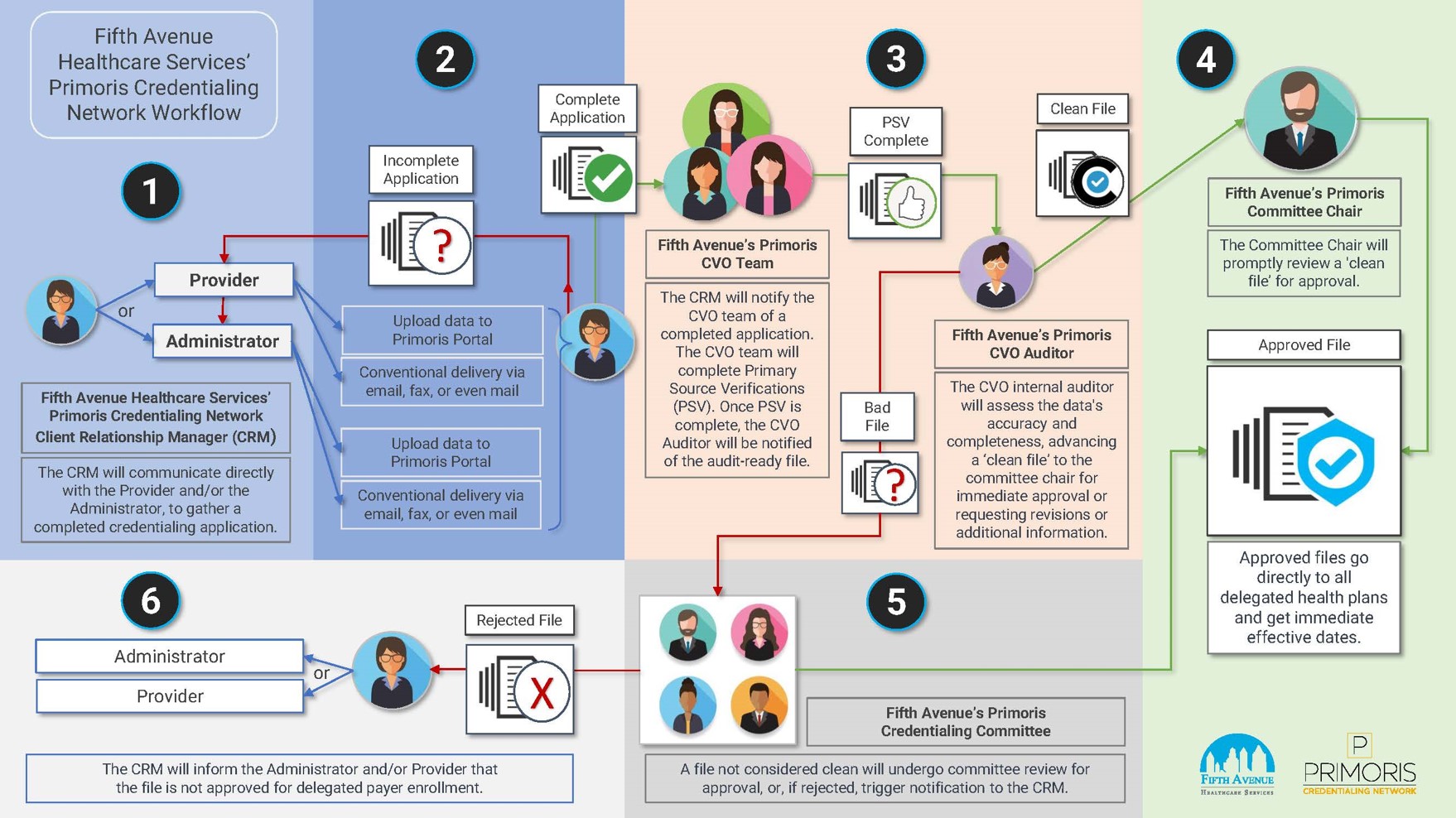
Automated credentialing workflows expedite application processing times, reduce manual errors, and enhance data accuracy. Machine learning algorithms can analyze credentialing data patterns to identify anomalies and flag potential compliance issues, enabling proactive risk management and quality assurance.
Source: The provider credentialing workflow displayed above is from Primoris Credentialing Network. Reports from healthcare technology research firms like KLAS Research or articles in publications like Healthcare IT News might discuss the adoption of automation technologies in credentialing.
6. Interoperable Credentialing Systems
Healthcare organizations are investing in interoperable credentialing systems that facilitate seamless data exchange between internal and external stakeholders. Interoperable systems enable healthcare entities to share credentialing data with health plans, regulatory agencies, and affiliated organizations in a standardized format.
By promoting data interoperability, healthcare organizations can enhance care coordination, facilitate provider network management, and improve regulatory reporting capabilities.
Source: Industry reports from organizations like HIMSS (Healthcare Information and Management Systems Society) or research articles in healthcare informatics journals could provide insights into interoperability trends.
7. Focus on Quality and Patient Safety Metrics
Credentialing criteria are evolving to incorporate quality and patient safety metrics as key indicators of provider performance. Healthcare organizations prioritize providers who demonstrate a commitment to delivering high-quality care and achieving positive patient outcomes.
Credentialing committees assess providers’ adherence to evidence-based practices, clinical performance metrics, patient satisfaction scores, and participation in quality improvement initiatives.
By aligning provider credentialing criteria with quality and safety objectives, healthcare organizations can enhance care quality, mitigate patient risks, and foster a culture of continuous improvement.
Source: Publications like the Agency for Healthcare Research and Quality (AHRQ) or academic journals focusing on patient safety and quality improvement may have additional relevant information.
8. Continued Education and Maintenance of Certification (MOC)
Healthcare organizations emphasize the importance of continued education and maintenance of certification for providers to stay abreast of evolving standards of care, technology advancements, and regulatory changes. Maintenance of certification programs requires providers to participate in ongoing professional development activities, demonstrate competency in their specialties, and periodically renew their certifications.

By promoting lifelong learning and professional growth, healthcare organizations ensure that providers deliver optimal care and uphold licensure requirements.
Source: Credentialing blogs from sources such as Fifth Avenue Healthcare Services’ credentialing blog and medical associations like the American Medical Association (AMA) or nursing associations frequently publish guidelines and recommendations for continuing education and certification maintenance.
9. Enhanced Peer Review Processes
Peer review committees play a vital role in evaluating provider competence, professionalism, and adherence to clinical standards. Healthcare organizations are enhancing peer review processes to ensure fairness, transparency, and consistency in assessing provider performance.
Peer review committees conduct comprehensive assessments of providers’ clinical outcomes, adherence to clinical guidelines, communication skills, and ethical conduct. By fostering a culture of peer accountability and constructive feedback, healthcare organizations can identify opportunities for performance improvement, mitigate clinical risks, and uphold patient safety standards.
Source: Resources from organizations like the American Board of Medical Specialties (ABMS) or academic journals on medical ethics and peer review processes might offer relevant insights.
10. Credentialing for Allied Health Professionals
Allied health professionals, including nurses, pharmacists, therapists, and technologists, play integral roles in healthcare delivery and patient care. Healthcare organizations are expanding credentialing initiatives to include allied health professionals, ensuring they meet competency requirements and adhere to scope of practice guidelines.
Credentialing criteria for allied health professionals encompass education, licensure, certification, and specialty training relevant to their respective disciplines. By credentialing allied health professionals, healthcare organizations enhance interdisciplinary collaboration, optimize care delivery processes, and maximize patient outcomes.
Source: Professional associations for allied health professions, such as the American Nurses Association (ANA) or the American Association of Medical Assistants (AAMA), often publish information on credentialing requirements and trends.
In conclusion, the evolution of provider credentialing in healthcare reflects a dynamic and multifaceted landscape shaped by technological innovation, regulatory imperatives, and quality-driven initiatives. As healthcare organizations strive to optimize credentialing processes, it is imperative to prioritize patient safety, care quality, and provider competence.
By embracing digital solutions, standardized practices, and evidence-based criteria, healthcare organizations can enhance their credentialing programs’ efficiency, effectiveness, and integrity. Continuing collaboration, innovation, and investment in credentialing excellence will be essential to meeting the evolving needs of patients, providers, and healthcare systems in an increasingly complex and interconnected healthcare environment.
More information about Fifth Avenue Healthcare Services
Fifth Avenue Healthcare Services is an NCQA Credentialing Accredited family of healthcare companies. Sister companies include 5ACVO (credentialing and primary source verification specialists), Fifth Avenue Agency (MPLI and medical malpractice insurance specialists), and Primoris Credentialing Network (credentialing and provider enrollment specialists with 54+ health plan and network provider enrollment options).
Fifth Avenue Healthcare Services initially published this article here. For information on Fifth Avenue Healthcare Services, please visit FifthAvenueHealthcareService.com or Contact Us.