A recent Medscape survey found that 31% of medical malpractice lawsuits stemmed from the failure to diagnose. 16% resulted from the failure to treat or delayed treatment. The poor documentation of patient instruction accounted for 4%. Although no one can be certain why these cases happened, what can be agreed upon is that following the fourth C of Medical Malpractice Prevention could have reduced these percentages.
Charting remains a simple, effective way to decrease medical malpractice in various healthcare settings. With premiums increasing, physicians can follow some of the best charting practices to help themselves and their patients.
The Goal of Charting
The primary objective of medical charting is to ensure that patients are adequately treated. Patient medical records typically include personal data, physical and mental condition information, medical history, and current medical care. Accurate documentation of patient medical records can help ensure that patients receive adequate treatment, which can reduce the number of medical malpractice claims physicians must deal with.
Patients and their physicians can use medical records to formulate and follow courses of treatment. Both parties can determine if prescribed treatments are working and adjust what is not by examining records. Additionally, medical records can help improve treatments for future patients by providing a blueprint of what worked and what did not.
Patient records can also be used to evaluate the quality of care in case of a medical malpractice claim and support ongoing medical research. A physician’s performance is all but captured in a patient’s records, especially if they are accurate and complete. A thorough reading of a patient’s records can show whether or not a physician’s treatment meets accepted standards. Therefore it is crucial for physicians to properly chart every patient they assist. Without patient records, researchers might find collecting data about medications, treatments, and outcomes more difficult. Records help researchers assess side effects and pursue new lines of thinking that may result in even better treatment.
Everything that happens to patients should be documented. Procedures, treatments, and instructions must be recorded. Following some of the best practices of medical charting can help patients, physicians, and the entire medical community.
3 Best Practices for Charting
1. Charting Best Practice: Follow the 6 C’s of Charting
All physicians should keep the 6 C’s of Charting in mind to maintain accurate and current patient medical records.
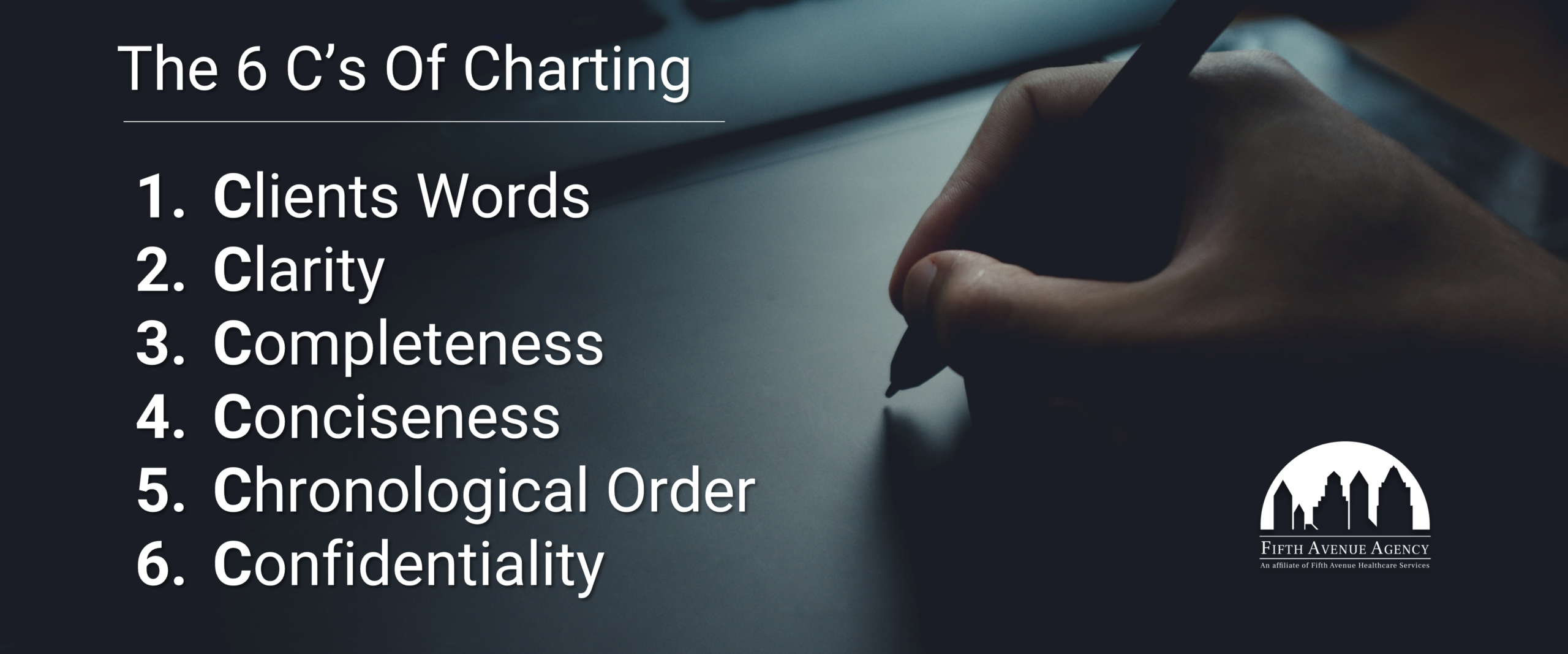
The 6 Cs of Charting includes using the following: Client’s Words, Clarity, Completeness, Conciseness, Chronological Order, and Confidentiality.
- Client’s Words: Patients can typically describe their symptoms best. Physicians can guess how patients feel, but the onus to describe their conditions rests on patients. As such, physicians should document exactly what their patients tell them. The patient’s exact words can help physicians make precise diagnoses. The patient’s words should not be rephrased or summarized. Whatever they say should be recorded in their chart.
- Clarity: Anyone with medical knowledge should read a patient’s chart. Physicians should use standard medical terminology to describe patients’ conditions to maintain continuity among everyone’s charts. Using accepted terms helps keep everyone on the same page when different physicians read the same chart.
- Completeness: Thorough documentation can go a long way when treating a patient. Information is power when it comes to the health care of an ailing person. Physicians should provide as much complete information as possible. This includes filling out all forms. Any gaps can cause treatment delays which can lead to further injuries.
- Conciseness: Although all charts should be complete, recorded information should be brief. Keeping documentation to the point can make scanning a chart quick and straightforward. Standard terminology and abbreviations can keep patients’ medical records concise and clear.
- Chronological Order: Documenting events as they happen can facilitate patient care and resolve any legal issues should they arise. Furthermore, dating every chart entry creates a timeline to help physicians pinpoint what went wrong. A chart that contains recorded events that are out of order can confuse anyone who reads it.
- Confidentiality: Medical data is among the most sensitive data that exists. All information in a patient’s medical record should be kept strictly confidential. Maintaining this bond of secrecy creates trust between patients and their physicians. Breaking it can have legal ramifications.
2. Charting Best Practice: Legible and Timely Charting
Legibility: Health care can be a hectic field. Physicians have much to deal with. Charting alone can be a huge ordeal. The last thing busy physicians probably want to deal with is ensuring their handwriting is legible. However, sloppy notes can create confusion and medical errors. Guessing what someone wrote can open up physicians and their practices to medical malpractice.
Fortunately, the agreed-upon use of medical terms and abbreviations can help offset sloppy penmanship. Also, medical transcription can transform scribbles into digital text, clearing up much of the chaos surrounding someone’s scrawl. Still, proper grammar and spelling can lay a solid foundation for a chart’s legibility.
Timeliness: Prolonged treatment can cause irreparable harm. Medical records must be kept up-to-date each step of the way to enable prompt health care. All exams and test results should be documented as soon as they are available. Even communication between physicians should be recorded in a timely fashion. Patient medical records should be as current as the patient’s condition. Physicians can make the most informed decisions with existing data at their disposal.
3. Charting Best Practice: The Golden Rule of Charting
Physicians should document everything. They should chart under the assumption using the Golden Rule of Charting, which states that if something was not documented, it did not happen.
Details can help patients and physicians should medical malpractice rear its head. If specific details are not documented, then it usually not be proven that an event occurred. All medical procedures, treatments, and instructions must be charted. Only facts should be recorded, not the opinions of physicians or others.
Bonus Charting Tips
Use EMR responsibly
Electronic medical record (EMR) systems can save time and eliminate much pain from charting. However, it can be too easy to select parameters and move on to the next record automatically. It is imperative that you do not abuse this feature. You must be deliberate when selecting information in EMR systems.
Tie up loose ends
When you record a patient complaint, that complaint must eventually be addressed in the chart. This includes multiple complaints from the same patient. While focusing on the main complaint is acceptable, each issue must be addressed, even if it means discussing them at the next visit.
Obtain and document consent
The Medscape survey found that 2% of medical malpractice claims were caused by improperly obtaining or lacking. Physicians can cover themselves by promptly acquiring consent and recording when. A signed consent should be included in every applicable chart.
Record refusal of care and non-compliance
Equally crucial as documenting consent is recording the refusal of care and non-compliance. If a patient refuses suggestions for their care, then the burden rests on physicians to document it. If the patient refuses recommendations and tries to sue for malpractice, physicians can present this documentation to help defend themselves.
Include follow-up instructions
Some physicians push their patients out the door without proper follow-up instructions. This tactic can prove harmful should a patient suffer an unfortunate setback. Providing follow-up instructions to patients and including a copy in their chart can help in litigation. Physicians can boost their documentation by inserting a printed copy of aftercare directions into a patient’s chart.
Edit records with caution
Medical records are legal documents. Changing the information they contain can have dire repercussions. If an error is found in a chart, then physicians can draw a line through it. One line can signify the mistake as well as sustain its legibility. Physicians who remember to add something to a chart after the fact can add the item and document their addendum by noting the date and time.
Be consistent
Using standard terminology and abbreviations is a surefire way to maintain consistency. Physicians with their notation or reminder system should stick with one system throughout their careers. Being consistent can reduce confusion and misinterpretations.
Chart for others
A final charting tip is that it might be best to chart for everyone else but yourself. Sure, you can understand your private notation system and your handwriting. What about those who take over once your shift ends? What about those who take over if you become incapacitated? Charting for others can help promote firm documentation for everyone who needs to read a record.
The 4 C’s of Medical Malpractice Prevention
1. Charting
2. Compassion
Compassion, or Caring, helps forge a relationship between physicians and their patients. Physicians can leverage this bond should one of their patients sue for malpractice. A patient who feels their physician is compassionate might be less likely to carry through on a malpractice claim.
Physicians can act compassionately in several ways. They can:
- Avoid criticism of other physicians.
- Be honest with the patient.
- Be mindful of nonverbal signals.
- Maintain good eye contact.
- Use the patient’s name whenever possible.
3. Communication
Charting ties into communication. Physicians might struggle with communicating treatments to their patients with poor charts. This can indeed lead to an unfortunate situation. Since incorrect and late information is primarily responsible for negligence, physicians must communicate with their patients with as much data as possible.
Physicians can practice effective communication when they:
- Clearly explain the situation.
- Encourage the patient to ask questions.
- Ensure the patient understands the issue and course of treatment.
- Listen to the patient’s concerns.
- Understand the patient’s point of view.
- Verify the accuracy of a diagnosis and treatment plan, including medication.
4. Competence
Physicians are expected to tender treatment per the standards of their peers. Simply put, they must know what to do and when to act. If one of their peers can perform a particular way, they can be expected to perform the same way. Adhering to the standards of their profession can go the distance when preventing medical malpractice.
Physicians aiming to demonstrate superior competence can:
- Double-check their work for any mistakes.
- Keep their skills updated within their field of medicine.
- Realize when a situation is beyond their expertise and seek outside guidance.
The Cost of Medical Malpractice
Physicians who refuse to take charting seriously risk injuring patients and damaging their careers. Medical malpractice can be an expensive lesson to learn. Not following any of the C’s of Medical Malpractice Prevention can expose physicians to costs they may never recover from.
A $205 Million Lesson
In July 2019, a Baltimore, Maryland jury awarded Erica Byrom $229 million when they determined her daughter suffered a brain injury during birth. The state cap decreased the damages to $205 million, making it the largest medical malpractice verdict in United States history. Incorrect information led to ill-informed decisions that resulted in the daughter needing constant care for the rest of her life.
A $135 Million Lesson
10-year-old Faith DeGrand was awarded $135 million when a jury found her back surgeon was responsible for paralyzing her during botched scoliosis surgery. Although DeGrand is only partially paralyzed, this negligence forever altered her life.
A $111 Million Lesson
Minnesota’s largest medical malpractice verdict in history happened in 2022 when a jury awarded $111 million to the plaintiff for failing to diagnose and properly treat the plaintiff for a leg injury. The plaintiff suffered muscle and nerve damage and could experience amputation, infection, renal failure, or death related to the malpractice.
Conclusion
Physicians ultimately have the power to reduce medical malpractice premiums and support physicians should an unexpected turn of events take place. When used with all the 4 C’s of Medical Malpractice Prevention, charting can be the perfect supplement in a physician’s medicine bag.
More information about Fifth Avenue Agency
Fifth Avenue Agency specializes in MPLI and medical malpractice insurance, serving 1000s of providers nationwide. Fifth Avenue Agency is part of the Fifth Avenue Healthcare Services family. Sister companies include 5ACVO (credentialing and primary source verification specialists) and Primoris Credentialing Network (credentialing and provider enrollment specialists with 54+ health plan and network provider enrollment options).
This article was initially published by Fifth Avenue Agency here. For information on Fifth Avenue Agency, please visit FifthAvenueAgency.com or Contact Us.